12 December 2024
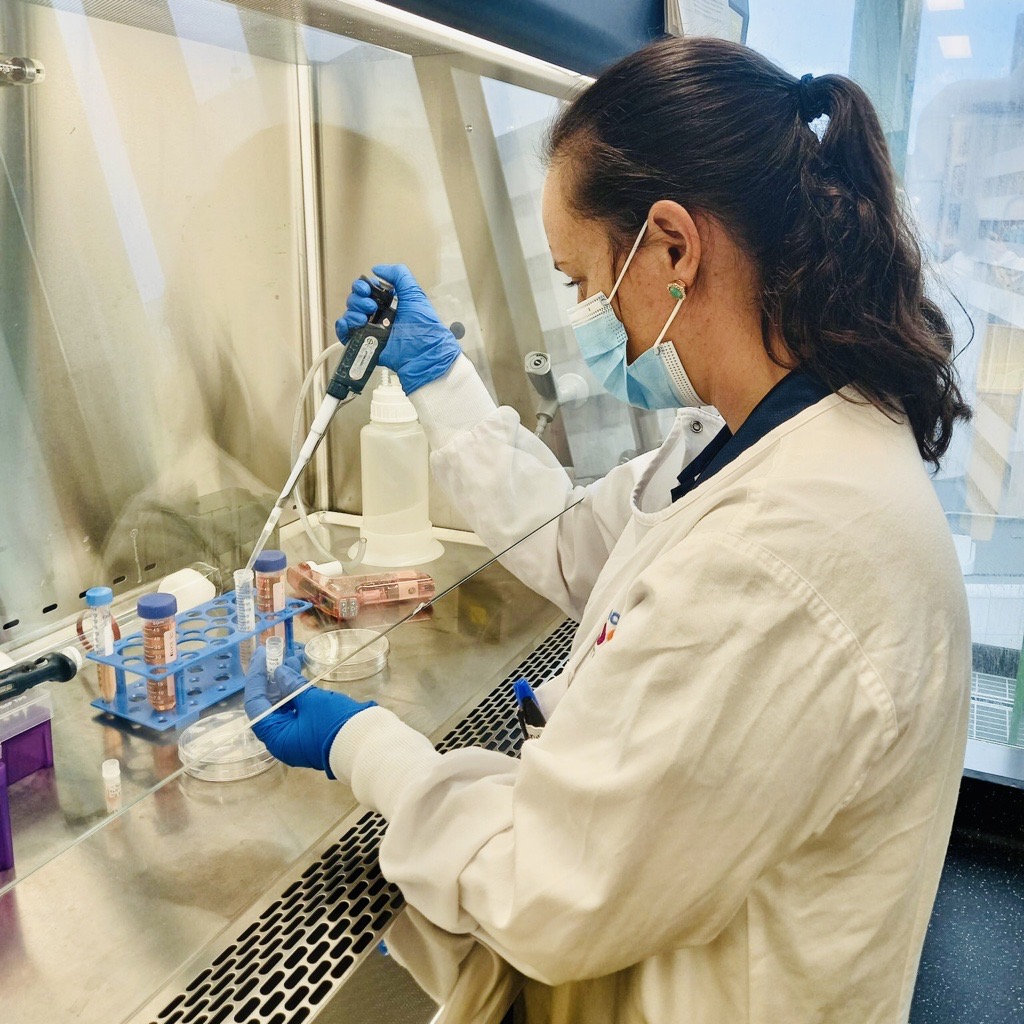
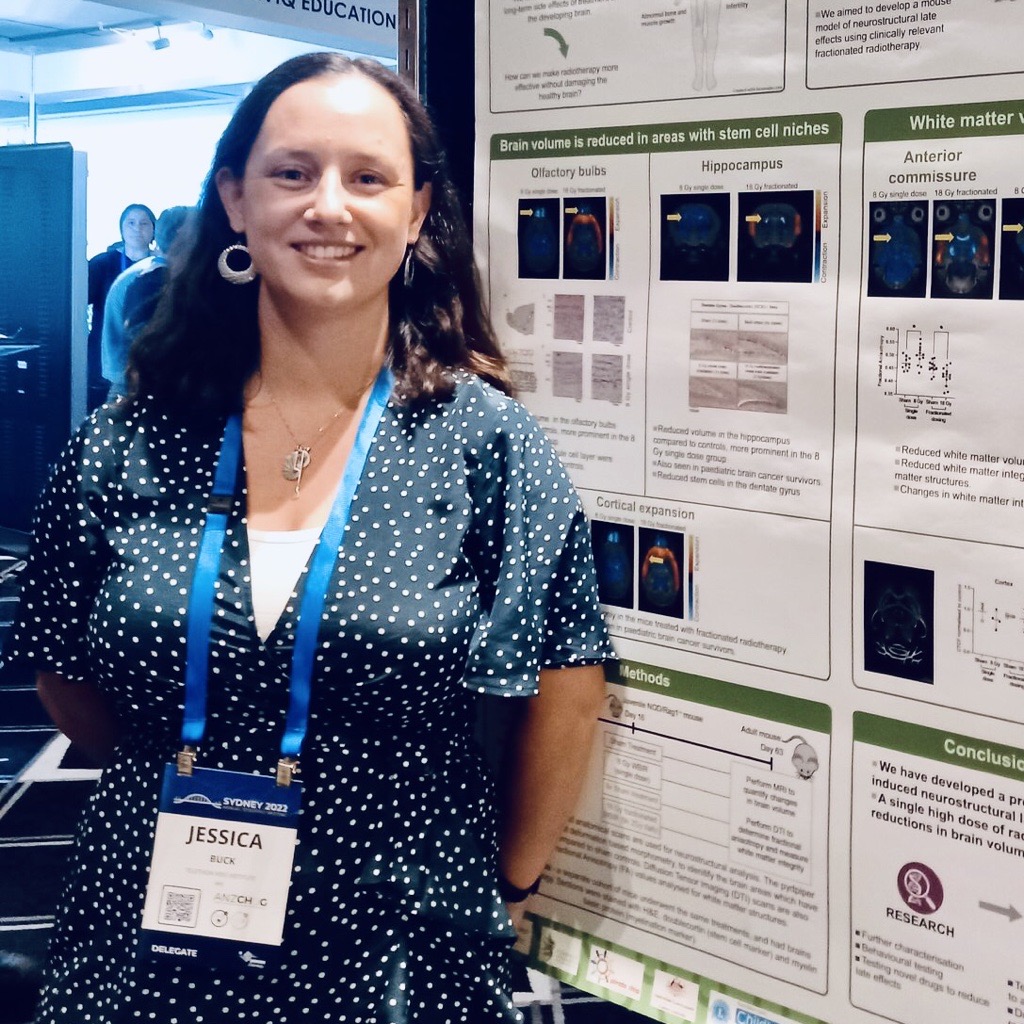
With the support of a AUD$199,445 Better Tools Grant from the Charlie Teo Foundation in 2022, Dr Jessica Buck and her research team in Perth, Australia, have made groundbreaking strides in the fight against childhood brain cancer.
About the Researcher
Dr Jessica Buck is a Senior Research Fellow at The Kids Research Institute Australia in Perth. One of ‘Australia’s Superstars of STEM’, proud Kamilaroi woman and the first Aboriginal woman to graduate with a PhD from Oxford, Charlie Teo Foundation funded Dr Buck locally to develop world-first tools in brain cancer.
We are also immensely proud to have funded and supported Dr Buck through her parental leave as she became a new mum!

“When I studied the human body at university, there were so many fascinating subjects that I couldn’t choose what I liked best. A friend suggested I combine my interests, which were neuroscience (study of the brain) and oncology (the study of cancer), so I chose to research brain cancer!
I completed my training in neuroscience and oncology at one of the top universities in the world, the University of Oxford. Now I’m back in Australia using my expertise to develop more effective, less toxic treatments for kids with brain cancer.
I was the first Aboriginal woman to graduate with a PhD from the University of Oxford. Ten years ago there had never been an Aboriginal person studying at Oxford or Cambridge. Now there are more than 40 of us, and we have the trailblazers who came before us to thank.
Aboriginal people are doing great things in mathematics, medicine, the arts, and the sciences. We are setting a path for the next generation of young Australians to follow, and I hope we can be successful in teaching and inspiring them to reach their potential, in cancer research or wherever that may lie."
Dr Jessica Buck, The Kids Research Institute Australia
Key Findings and Impact of this Research Grant
Brain cancer remains the leading cause of disease-related death in Australian children, and current treatments like radiotherapy and chemotherapy often fall short. This is in part due to how preclinical testing is performed, where many treatment options for children are only tested on adult preclinical models. This completely ignores differences that exist between adults and children in the developmental stage of their brain, immune system, other organs, and tumour microenvironment.
To address this, Dr Buck’s team developed the world’s first child-specific paediatric mouse models that mimic the way children’s bodies and immune systems develop.
One of the key findings from this research is that medulloblastoma, the most common childhood brain cancer, grows more rapidly in paediatric mice than in adult mice. Additionally, paediatric mice have fewer immune cells in their tumours compared to adults, highlighting the need for treatments tailored specifically for children. These disparities between paediatric and adult mice further highlight the importance of using biologically representative preclinical models in research.
Using these new models, the team identified new immunotherapy options that boost children’s immune systems to fight cancer more effectively. For instance, they found that radiation therapy, while less effective in paediatric models, increases the number of “cancer-eating” immune cells which could be leveraged for the development of paediatric-specific immunotherapies. This discovery is akin to finding a new way to train the body’s own soldiers to better fight off invaders.
The impact of this research extends far beyond the lab. These innovative models have been embedded within the Kids Research Institute Australia’s strategic plan, attracting over $2 million in additional funding. The program now involves five research teams and has trained more than ten students and researchers in performing highly technical procedures.
To further validate their findings, Dr Buck’s team has established active collaborations with two international research teams led by world-renowned experts in paediatric cancer from Cambridge University and McGill University. These collaborations strengthen the research and ensure its relevance to human patient datasets.

Looking ahead, Dr Buck’s team aims to use this research as the foundation for paediatric brain cancer-specific immunotherapy clinical trials. This ambitious goal holds the promise of significantly improving brain cancer survival rates and providing new hope to children and their families.
“Survival rates for kids with brain cancer have barely changed in 30 years. The treatments we use haven’t changed either…
To date very few new brain cancer drugs have been identified for children. We believe this is partially because children are treated as ‘small adults’ in cancer drug discovery. Virtually all pre-clinical studies are conducted in adult models rather than paediatric models.
This completely ignores massive differences that exist between adults and children in the developmental stage of their brain, immune system, organs, and tumour microenvironment.
Under my Charlie Teo Foundation Grant, I developed world-first techniques to more accurately evaluate new childhood brain cancer therapies. Our pipeline aims to enable the testing of new immunotherapies in paediatric models for the first time.
We desperately need more research into this devastating disease to develop better treatments. This is why charities like the Charlie Teo Foundation are SO important. Better research can provide HOPE to kids with brain cancer and their families.”
Dr Jessica Buck, The Kids Research Institute Australia
12 December 2024
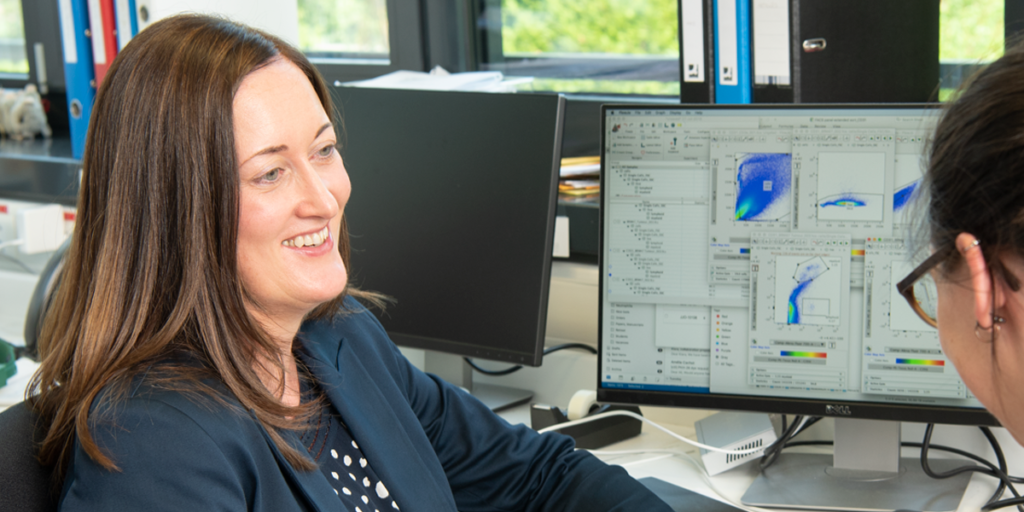
Prof Johanna Joyce was awarded a AUD$200,000 Research Rebel grant in 2021 from the Charlie Teo Foundation which supported her courageous and creative brain cancer research laboratory. Over the past two years, the Joyce Lab has made significant strides in advancing the brain cancer field and their work has led to the publication of six high-impact papers, unveiling groundbreaking findings that offer meaningful hope for patients.

Prof Joyce’s research has focused on the tumour microenvironment (TME), which can be imagined as the “neighbourhood” where cancer cells live. Her lab is a world expert in developing and leveraging high resolution microscopy techniques to literally ‘look inside’ the brain of living animals over time to understand how brain tumours develop and the role that the TME plays in cancer growth. In the context of brain cancer, the TME has a significant impact on the behaviour and spread of cancer cells, much like how the dynamics of a neighbourhood can influence the behaviour of its residents. By understanding this neighbourhood better, scientists can find new ways to disrupt the activities of cancer cells and prevent them from spreading.

One of the standout discoveries includes a non-invasive technique using Fluorine-19 MRI to monitor tumour-associated macrophages, which are like the “watchdogs” of the tumour neighbourhood as they can surveil and influence tumour progression. Monitoring these watchdogs have been traditionally achieved through invasive biopsies. This new technique allows doctors to keep an eye on these watchdogs without needing invasive biopsies, making it easier to track how brain tumours are behaving and responding to treatment. These findings were published in the prestigious journal Scientific Translational Medicine
Another major advancement is the creation of a multimodal imaging strategy that combines MRI and two-photon microscopy. Think of this as using both a telescope and a microscope to study the same area. This approach has revealed how these watchdogs move and interact with the tumour over time, helping scientists understand how different treatments affect the tumour environment, and ultimately how this affects the invasiveness of brain tumours. These findings were published in the prestigious journal iScience
Prof Joyce’s team also introduced a novel imaging platform that enables researchers to perform detailed investigations of brain cancer progression over time, which was not possible before. This protocol was published in STAR protocols
Additionally, the Joyce Lab identified specific types of immune cells called macrophages in the tumour environment that play an important role in brain metastases. This is akin to discovering which specific neighbours in the TME are aiding the metastases of cancer cells, allowing researchers to devise strategies to target them directly with new treatments. These key findings were published in iScience
Additionally, their work on a new technique called Hyperplexed Immunofluorescence Imaging (HIFI) has enhanced the understanding of how tumours respond to radiation therapy. The advancement of this technique is analogous to upgrading from a black-and-white map to a detailed, colourful one. HIFI allows scientists to see over 45 different features in delicate tissue samples at high magnification, all at once. This technique, combined with advanced machine learning and network analysis, helps researchers understand how different parts of the tumour city respond to radiation therapy and provides insight into how we can tailor therapies more effectively. These key findings were published in Nature Communications
Finally, the Joyce Lab has uncovered a new role of fibrotic scars in promoting brain tumour survival and recurrence. These scars act like “safe houses” for glioma cancer cells, providing them shelter and helping them survive treatments. By targeting these safe houses, new treatment strategies could prevent the cancer from coming back. These findings have been published in Cancer Cell
These collective advancements not only deepen our understanding of brain cancer progression but also pave the way for more effective, personalised treatments. The innovative diagnostic tools and targeted therapies emerging from Prof Joyce’s research laboratory hold great promise for enhancing patient survival rates and quality of life. We commend Prof Joyce for such an outstanding research program and are thrilled to have supported her truly game-changing research.
“We published a total of six papers from this research program, supported in part thanks to the generosity of the Charlie Teo Foundation. I would like to take this opportunity to again thank you all at the foundation, with the shared mission of advancing knowledge to help the treatment of brain cancers."
Prof. Johanna Joyce, University of Lausanne, Switzerland
12 December 2024
Charlie Teo Foundation has invested over AUD$1 million to support scientists at Northwestern University to build Better Tools to treat brain cancer.
One of these courageous scientists is Craig Horbinski, M.D., PhD, director of Neuropathology at Northwestern Medicine and part of the team at Malnati Brain Tumor Institute at Northwestern.
Key Findings and Impact of this Research Grant
We’re excited to announce the latest progress from Prof. Craig Horbinski, a recipient of a $275,860 AUD Better Tools grant from the Charlie Teo Foundation. Prof. Horbinski is leading groundbreaking research to develop new ways to diagnose paediatric brain cancer using just a blood sample, reducing the need for invasive surgical biopsies. His team’s findings, recently published in the high-impact journal Acta Neuropathologica, bring hope for more accurate and less complex ways to detect brain tumours in children.

The team’s approach uses a methodology called a liquid biopsy, which works by searching for tiny bits of DNA that tumours shed into the bloodstream. Think of the tumour as a tree, and these fragments of cell-free DNA are like leaves that fall into a river. By collecting and analysing a blood sample, doctors can catch and study these “leaves” which can provide important clues about the tumour, all without needing to touch the brain.
In the study, Prof. Horbinski’s team examined blood samples from 77 children with brain tumours and compared them to blood samples from 16 children without tumours. They developed a blood test that can detect different types of brain tumours by identifying specific patterns in the DNA shed by the cancer cells—kind of like finding the fingerprints of a criminal at a crime scene. By developing machine learning algorithms to look at these patterns, researchers can help detect and potentially diagnose brain tumours without going inside the brain. Incredibly, they were able to distinguish children with brain tumours from those without with 83% accuracy from just a blood sample.

When it came to specific tumour types, the test worked particularly well. For circumscribed astrocytic glioma and glioneuronal tumours, it accurately distinguished these tumours from non-cancerous conditions in 86% and 83% of cases respectively.
To the best of our knowledge, this is the world’s first study to show that a blood test could aid in diagnosing children suspected of having a brain tumour. While the test demonstrated significant promise for certain tumour types, it was less effective for others, likely due to the complex and varied nature of brain tumours. For the two main subtypes—circumscribed astrocytic glioma and glioneuronal tumours—the test achieved a solid 80% accuracy. However, it had lower performance for rarer brain tumour types and may need further refinement and a larger sample size to provide statistically reliable results for these less common tumours.
Although the test showed strong potential, in the interim the researchers caution that it is not yet perfect and cannot replace traditional diagnostic tools such as brain scans or surgery. Nevertheless, this approach could be a valuable addition to presurgical evaluations, providing doctors with critical information to help guide treatment decisions.
Thanks to your generosity, your support of the Charlie Teo Foundation is driving innovation that can transform how we detect and treat paediatric brain cancer. Together, we’re making a real impact and bringing real hope for faster, safer diagnoses and improved outcomes. Please consider donating to the Charlie Teo Foundation to help advance research like Prof. Horbinski’s.
Dr Peter Truong - Head of Research
12 December 2024
Supported by a AUD$295,278 Better Tools Grant from the Charlie Teo Foundation, A/Prof. David Cormode and A/Prof Jay Dorsey, and their laboratories have made significant strides in developing local drug delivery for GBM with a cutting-edge technique called FLASH radiotherapy.
GBM has an average life expectancy of just 15 months, making the need for new treatments urgent.
A/Prof. Cormode’s and A/Prof Jay Dorsey’s research focuses on using a radiation-responsive drug-loaded hydrogel, a soft, drug-infused polymer that can be administered directly to the tumour site after surgery. This hydrogel acts like a sponge, slowly releasing the drug over time, and can release drugs in response to radiotherapy.
When combined with FLASH radiotherapy—a lightning-fast radiation treatment that takes only about a second—the results were remarkable: 86% of the immunocompetent mice treated with this combination survived to the end of the study, compared to none in the control groups (untreated, FLASH alone, or hydrogel alone).
This novel approach ensures high concentrations of drugs are delivered directly to the target site, while avoiding unnecessary systemic doses to other organs. Additionally, patients would require fewer healthcare visits since FLASH radiotherapy is administered in just a few sessions, with the hydrogel releasing the drug over time.

Key Findings and Impact of this Research Grant
One of the key achievements of this research was demonstrating the safety and effectiveness of this combination therapy in an immunocompetent model of GBM. This means the treatment was tested in a model that closely mimics the human immune system, making the findings highly relevant for future clinical applications.
The impact of this research extends beyond the lab. The project has served as a launchpad for two additional directions. First, the team is studying the use of SpaceOAR, an FDA-approved hydrogel, as a drug delivery vehicle. This hydrogel can be loaded with nanoparticles and drugs, which are then released to kill GBM cells. Second, they are exploring the combination of local drug administration with CAR T-cell therapy, a promising immunotherapy approach. By locally administering chemicals that attract immune cells, they aim to enhance the accumulation and activation of CAR T-cells, improving therapeutic outcomes.
22 October 2024
Charlie Teo Foundation funded researcher Prof Matt Dun today gave the televised National Press Club address in Canberra, and was presented with the 2024 Australian Society for Medical Research (ASMR) Medal.


Our CEO Alana Phadke was honoured to attend the National Press Club of Australia as a guest of the University of Newcastle together with representatives of Prof Dun’s philanthropic funders including RUN DIPG, Little Legs Foundation, The Kids’ Cancer Project, Isabella and Marcus Foundation and Rare Cancers Australia.
We are proud that Charlie Teo Foundation’s philanthropic support of close to $2 million has enabled Prof Dun’s exceptional brain cancer research and advocacy work being recognised today on a national level!

Matt is a man on a mission. He shared his experience as a scientist who dedicated his life to DIPG research when his daughter Josie was diagnosed with DIPG in 2018. Josie passed away 22 months post-diagnosis, forever 4 years old. We heard stories of HOPE and PROGRESS being made in DIPG/DMG research. We passionately share Matt’s plea that all of this is only possible if vital brain cancer research receives MORE FUNDING.

We are honoured to fund scientists like Prof Dun who display courage and humanity in their quest for a cure. Thank you, Prof Dun, for your recognition of Charlie Teo Foundation’s funding in your national address – to our supporters and donors, we could not do this without you!
Thank you also to University of Newcastle for acknowledging Charlie Teo Foundation’s funding of Prof Dun’s ambitious research into DIPG/DMG. We are immensely proud to work together to save our children’s lives.
“University of Newcastle is honoured to thank you for the generous support of the Charlie Teo Foundation to continue the ambitious I-DIMENSIONS project.
As you know, we believe this project represents an important step forward in our understanding of, and ability to effectively treat, DMG tumours. Your support is vital to completing this crucial piece of work.
Thank you for being part of our strong community of friends, alumni, staff and student supporters who are united to help those in need. Together, we can change lives and create a better future for generations to come.”
University of Newcastle, Australia

Charlie Teo Foundation acknowledges the Traditional Owners of the lands where we work and their continuing connection to land, waters and community. We pay our respects to the people, the cultures and the Elders past, present and emerging.