A team of investigators led by Amy Heimberger, MD, PhD, just published new findings in the Journal of Clinical Investigation!
Charlie Teo Foundation is proud to have supported this groundbreaking research through a AU$500,000 Better Tools grant at Northwestern University, USA.

Charlie Teo Foundation held our research showcase in collaboration with the Garvan Institute of Medical Research in March 2024 to highlight the outcomes of our brain cancer research partnership over the last five years.

Charlie Teo Foundation Chair, Garry Browne AM, warmly welcomed our guests. We were proud to celebrate this work at our recent research showcase generously hosted by Garvan. We warmly welcomed scientists and supporters from Garvan and other research teams including University of New South Wales, University of Sydney, University of Technology, Sydney and University of Newcastle. We were honoured to have join us neurosurgeons, neurooncologists and neuropathologists from the St Vincent’s/Garvan network.

Charlie Teo Foundation CEO Alana Phadke opened the showcase by thanking all the scientists and clinicians working together to improve outcomes for people with brain cancer.

Professor Joseph Powell, Director of Translational Genomics at the Garvan Institute, was travelling overseas, virtually shared an important update and his vision for the future.

Joseph elaborated, “We started by generating an atlas of single-cell genomic data for brain tumours. This is the largest resource of its type in the world and is used by many researchers locally and globally.
That enabled us to move forward and develop computational and wet lab techniques to identify glioma stem cells (the origin cells in diffuse gliomas) and identify the genomic underpinnings of those cells that we think we can start targeting with new therapies.
Moving towards the future, we are looking at pre-clinical work—both for evaluating the role and impact of current therapies and for what we can do to start thinking about developing new therapies for diffuse gliomas.
This is something we are proud to continue in our lab at Garvan in collaboration with the Charlie Teo Foundation.” – Professor Powell

Dr Ashraf Zaman, a Garvan Research and Biobank Scientist, took guests on a deep dive into the team’s work and its future direction.
We were honoured to round off the evening with sincere thanks to everyone involved from Dr Charlie Teo AM.






14 December 2023 – Read Now

4 October 2023, updated 7 June 2024
Charlie Teo Foundation (CTF) has been made aware of online advertising scams that are illegally using our founder’s image and/or endorsement to promote alleged medications.
These scam ads use fake AI-generated images of Dr Charlie Teo on social media and website advertising. Dr Charlie Teo or CTF are not responsible for these fake online public advertisements, and we do not endorse or support them.
Dr Charlie Teo does not endorse or promote any medications in public advertising.
Many supporters have sent us copies of these online ads asking if they’re scams. The answer is yes. If you receive or see one of these fake ads, we urge you to report it. Please do not click on any ad links or provide your personal details.
The Australian Government provides information on how to report scams: https://www.cyber.gov.au/learn-basics/explore-basics/recognise-and-report-scams
19 September 2023
Today we pay special tribute to our little friend Alegra. Today would have been Alegra’s 12th birthday. A beautiful angel, taken too soon, age six.
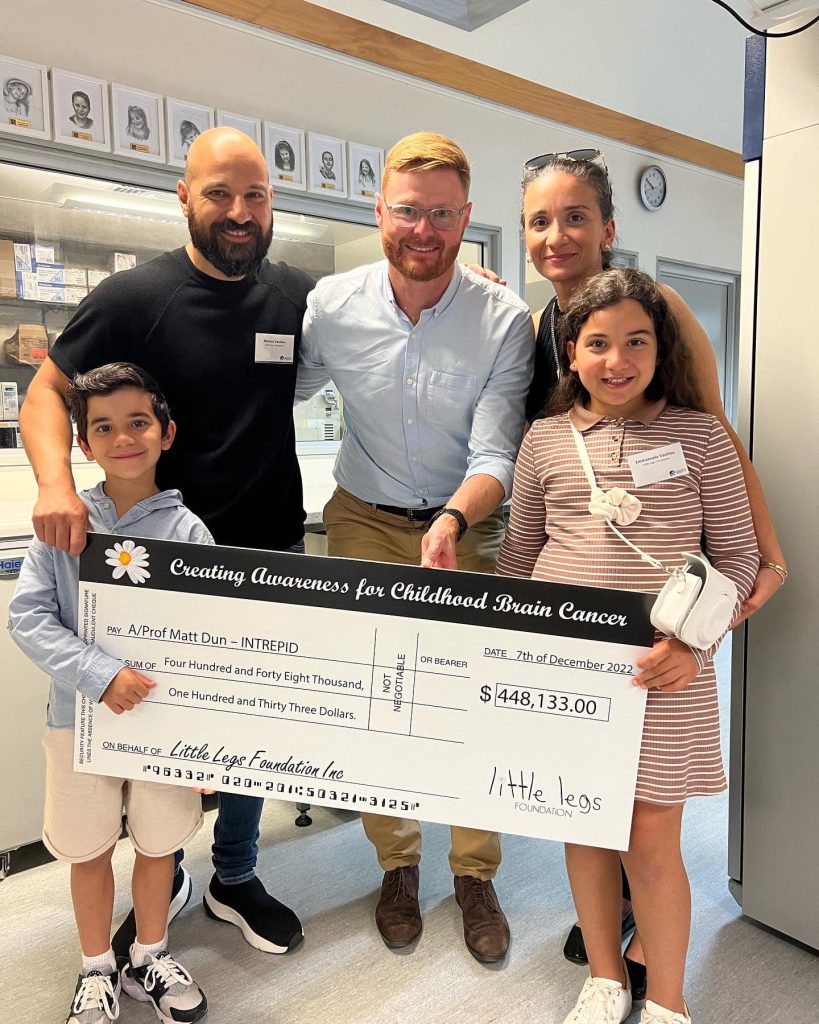
The Alegra’s Army Grant was established by the Little Legs Foundation in partnership with the Charlie Teo Foundation to ensure that no family and child has to suffer the ultimate price like Alegra.
We are proud today to honour Alegra by sharing recent DIPG research progress across the world.

Lethal, inoperable, and seemingly incurable – these are the sombre labels that have long characterised Diffuse Midline Gliomas (DMG), previously known as Diffuse Intrinsic Pontine Gliomas (DIPG).
DMG is a fatal type of cancer that predominantly affects children’s brain and spinal cords.
Unlike many other solid paediatric cancers, DMG doesn’t grow as large masses; instead, these cancer cells blend into healthy tissue, making them highly evasive and difficult to treat. The current treatment approach is palliative radiotherapy, bringing only short-lived relief, with patients often surviving just 9 to 11 months after diagnosis.
Here is where HOPE enters the picture….
Published findings from a team at Michigan University and international collaborators including Charlie Teo Foundation-funded superstar Professor Matt Dun, have shown for the first time in clinical trials that a new compound called ONC201 nearly doubled survival for patients with DMG compared to previous patients. This breakthrough cracks the seemingly unbreakable armour of DMG.
Prof Dun’s team didn’t stop there… They also figured out how DMG becomes resistant to ONC201 and found a way to tackle it. By combining ONC201 with another drug, ‘paxalisib,’ and standard radiotherapy, they’re aiming to boost the treatment’s effectiveness. These preclinical findings generated by Prof Matt Dun and his University of Newcastle research team supported the rationale for a DMG clinical trial known as PNOC022 that was recently brought to Australia, to test this combination therapy in DMG patients. Read more

Through the Charlie Teo Foundation’s More Data grant scheme, Prof Matt Dun and his team have also uncovered that ONC201 can potentially empower the immune system to better recognise and attack DMG cells. Empowering and engineering the immune system to better recognise and attack cancer cells has been shown to be effective and even curative in some forms of leukemia. However, this strategy remains quite difficult to implement in solid tumours like DIPG for a plethora of reasons which have been recently summarized by Dun Lab superstar, PhD candidate Bryce Thomas (supported by an Alegra’s Army PhD Scholarship), in the prestigious journal Trends in Cancer.

One of the main reasons DMG is so hard to tackle is because the tumour creates an environment around itself that shields it from the body’s immune system. This means that the immune system, which normally fights off infections and diseases, can’t effectively recognise and attack the cancer cells. This protective shield is made up of certain cells that are meant to help us, but in this case, they end up aiding the cancer’s growth.
Preliminary findings from Prof Matt Dun’s Alegra’s Army Grant funded in partnership with the Little Legs Foundation has shown that ONC201 can potentially weaken this protective shield, making the DMG cells more visible to the immune system and promoting an influx of battle-ready immune cells into the tumour. Further validation of this work is currently underway as the lab perfect the best DMG model to study the phenomenon in the lab. The Dun Lab suggests that a possible alternative treatment can include the use of ONC201 in combination with another type of immunotherapy called adoptive cell therapy or a chimeric antigen receptor (CAR) T cell therapy. This innovative approach involves modifying a patient’s own immune cells, teaching them to specifically target the DMG cancer cells.

Preliminary evidence from a Stanford study has shown that this approach demonstrated enhanced tumour reduction and improved neurological conditions in three of four patients.
However, an ongoing challenge associated with this strategy involves teaching the cells what DMG cells look like because not every DMG cell looks alike. From this project, Prof Matt Dun’s team have identified a potential marker that can better identify and differentiate DMG cells from healthy cells. The group are currently working on a strategy to exploit the finding in the clinical setting.
In the end, this isn’t just about science—it’s about HOPE. Prof Dun and his team are at the forefront, driving progress and uniting the masses. Their ONC201 breakthrough brightens the path ahead, reminding us that even in the face of the toughest challenges, science’s light can guide us toward solutions we once thought were beyond our grasp.

Brain cancer research is significantly underfunded compared to other cancers, meaning survival rates have barely improved in about 40 years. Research funders like the Charlie Teo Foundation are crucial to changing the future for brain cancer patients and families.
To date Charlie Teo Foundation has committed more than $10 million to brain cancer research in Australia and globally. This includes $2.7 million awarded into DIPG/DMG specific research. Compare this to the Australian Government that has awarded $970,000 to DIPG/DMG specific research over that same period.
United together we can shine a bright light on the need for more funding for brain cancer research and better treatments in Australia.
Charlie Teo Foundation acknowledges the Traditional Owners of the lands where we work and their continuing connection to land, waters and community. We pay our respects to the people, the cultures and the Elders past, present and emerging.
These terms and conditions (Terms) govern your use of this website located atwww.charlieteofoundation.org.au(Site). Throughout these Terms, when we mention ‘we’, ‘our’ or ‘us’, we mean Charlie Teo Foundation of Level 1, 605 Botany Rd, Rosebery NSW 2018.
Acceptance
Please read these Terms carefully before using this Site. By using this Site, you agree to be bound by these Terms. If you do not wish to be bound by these Terms, you should not use this Site and you should close this Site immediately.
We may revise these Terms from time to time. Revised Terms are effective immediately upon being posted onto this Site. Your continued use of this Site will mark your acceptance of any such revised Terms.
Use of Content
Unless otherwise indicated by us, we own all intellectual property rights, including copyright, in all text, graphics, images, artwork, photographs, pictures, trade marks, logos, computer code and other materials posted on this Site (Content), and the arrangement of this Content.
Occasionally, we may publish Content in which the copyright is not owned by us. When this is done, we make every effort to acknowledge the copyright owner.
The Content may only be used by you for personal, educational and non-commercial purposes. You agree not to:
(a) alter or remove any copyright, trade mark or other proprietary notice of ours or of any other company appearing on this Site;
(b) copy, sell, reproduce, republish, transmit or distribute, the Content or upload, post or display the Content on any other website or medium for publication or distribution or for any commercial enterprise;
(c) modify or edit the Content in any way; or
(d) to the maximum extent permitted by law, reverse engineer, translate, adapt or modify any software used in connection with this Site.
Our approval of any fundraising activity does not constitute permission to reproduce or modify any of the Content on this Site and all requests for such permission must be approved by us in writing.
The Content on this Site is for general information purposes only. We make no warranties or representations about the accuracy, reliability, currency or continuous supply of any of the Content on this Site. As a user of this Site, you are required to make your own enquiries before entering into any transaction on the basis of, or in reliance upon, the Content.
In the event that you find any inaccurate information on this Site, or have any complaint about what we have published, please emailinfo@charlieteofoundation.org.au. We will investigate the matter on receipt of your email and will take such further action as we consider appropriate.
Approved Instagram content terms and conditions
When accepting rights requests you are allowing the Charlie Teo Foundation to use your content in future marketing campaigns with no copyright.
Rights will be requested by the Charlie Teo Foundation via commenting on your Instagram or via a Tweet and require a response to approve use of your content. To agree to the Charlie Teo Foundation reusing your content simply reply using the hashtag #YesCharlieTeoFoundation
Copyright: Upon approval, photos become available for use by the Charlie Teo Foundation and each participant relinquishes any claims of ownership or rights therein upon approval of their content to be used.
Your Conduct
You must use this Site for lawful purposes only. You must not transmit via this Site any material which is illegal, threatening, abusive, defamatory, invasive of privacy rights, vulgar, obscene, profane or otherwise objectionable or inappropriate, or which violates or infringes in any way upon the rights of others.
Donations
Access to the Charlie Teo Foundation’s website including the “Donations” web page, is provided “as is” and “as available” and without warranty of any kind except those not able to be excluded by Australian law. Charlie Teo Foundation does not guarantee such access, particularly access by mobile phone, or that such access will be continuous, uninterrupted or secure. Mobile phone access to the website is subject to network limitations and availability as well as factors beyond the control of the Charlie Teo Foundation.
Other Terms and Conditions
Additional terms and conditions may apply to specific portions or features of this Site, including contests, promotions or other similar features, all of which terms are made a part of these Terms by this clause.
You agree to abide by such other terms and conditions, including (where applicable) representing that you are of sufficient legal age to use or participate in such service or feature. If there is a conflict between these Terms and the terms posted for, or applicable to, a specific portion of this Site or for any service offered on or through this Site, the latter terms will take precedence with respect to your use of that portion of this Site or the specific service.
Liability
Your access to and use of this Site is provided on an “as is” and “as available” basis.
To the full extent permitted by law, we disclaim all conditions, warranties or rights of any kind in relation to products, including, but not limited to, all implied warranties of merchantability, fitness for a particular purpose and non-infringement.
We are not responsible for any loss or damage caused by this Site (or a part of this Site) being suspended, terminated or your access to and use of this Site limited, or for late delivery or cancellation of an order of a product, except as set out expressly in these Terms.
While we exercise all due care, we cannot and do not guarantee or warrant that the Site will be free of infection, viruses, defects, harmful components or any other codes that may have contaminating or destructive properties. We recommend that you install up-to-date virus protection software on your computer prior to using this Site.
We also make no warranty that:
(a) the Site or products which you order through the Site will meet your requirements;
(b) the Site will be uninterrupted, timely, secure, or error-free; or
(c) the quality of any products, services, information, or other material purchased or obtained by you through the Site will meet your expectations.
Where any condition, warranty or right is implied by law and cannot be excluded, we limit our liability for breach of, or other act contrary to, that implied condition, warranty or right, at our option, to either:
(a) the re-supply of the products or services; or
(b) an amount equivalent to having the products or services re-supplied.
Except as expressly stated in these Terms and in respect of any liability that cannot be excluded by law, we will not be liable for any loss or damages of any kind (including any direct, indirect, incidental and consequential loss or damages) arising in connection with your access to, or use of, or inability to use this Site, the Content (including linked websites) or products which you order through this Site. The foregoing applies whether such loss or damages arise under contract, in tort, in negligence, under statute or otherwise.
Indemnity
We rely on you observing these Terms at all times. You agree to indemnify and hold us and our officers, employees and agents harmless from any claims of any nature whatsoever (including legal costs) by any third party arising out of or in connection with your access to and use of the Site. The indemnity is this clause extends to and covers your breach of these Terms.
Third Party Sites
We may link this Site to other websites which are not under the control of, or maintained by, us. We are providing these links to you only as a matter of convenience and, to the maximum extent permitted by law, we are not responsible for the content of such websites. We do not endorse or recommend any products, materials or services displayed or offered on any websites which may be linked to this Site.
Links from External Sites
We may grant you permission to create a hyperlink from any other website to this Site, upon request. You must receive our permission in writing prior to posting such a hyperlink.
All hyperlinks to this Site must point towww.charlieteofoundation.org.auand not to any internal page, and any text-only link must be identified as ‘Charlie Teo Foundation’. Any deviation from these Terms must be approved by us in writing.
Privacy
We are committed to respecting and protecting your personal information. Please refer to our Privacy Policy available on our website to learn more about how we handle personal information. Should you have any questions in relation to our Privacy Policy please email info@charlieteofoundation.org.au
General
These Terms between you and us will be governed by the laws of New South Wales, Australia. You agree that any dispute or legal proceeding in relation to this Site shall be brought exclusively in the courts of New South Wales, Australia.
Although this Site can be accessed throughout Australia and overseas, we do not represent that the content of this Site complies with the laws (including the intellectual property laws) of countries outside Australia. If you access this Site from outside Australia, you do this at your own risk and are responsible for ensuring compliance with all laws in the place where you are located.
If any provision or part of a provision of these Terms is held by a court of competent jurisdiction to be contrary to law, all other provisions shall remain in full force and effect.
These Terms comprise the entire agreement between you and us in respect to your use of this Site.
Last updated December 2019
This Privacy Policy sets out our commitment to protecting the privacy of your personal information in accordance with the Privacy Act 1988 (Cth) and the Australian Privacy Principles. Charlie Teo Foundation ABN 57 622 041 061 only collects personal information that is reasonably necessary for us to perform our charitable activities.
What is personal information?
Personal information is information or an opinion about an identified individual, or an individual that is reasonably identifiable. Personal information can include a person’s name, address, contact details, date of birth, gender, sexuality and race.
What personal information does Charlie Teo Foundation collect and why?
To enable us to undertake our charitable activities we may collect the following personal information from you:
• Your name, title, signature, address, phone number, email, date of birth and employment details;
• Health information;
• Payment and billing details including bank and credit card details.
If you are making a donation, we may also ask you to provide details about the motivation for the gift and whether it is made on behalf of an individual or an organisation.
Who do we collect personal information from?
Charlie Teo Foundation may collect personal information from donors, volunteers, fundraisers, people with or affected by brain cancer, event guests, corporate partners and sponsors,researchers and research institutions, grantees, suppliers, service providers and other supporters.
How do we collect your personal information?
We may collect personal informationfrom you in various ways, including in-person, by telephone, via our website or email, the internet, through social media or by mail.
Third parties might also collect personal information from you (for example, organisers of fundraisers) to provide to us.
What do we do with your personal information?
Charlie Teo Foundation uses personal information in the following ways:
• To communicate with you about our activities including but not limited to upcoming fundraising events, campaigns, research activities and outcomes;
• To process your donation or application to organise a fundraiser;
• To enable us to undertake our volunteer program;
• For marketing and promotion of our activities including to help raise awareness and funds for brain cancer research;
• To enable us to conduct our grant program and research activities; and
• To comply with legislative or regulatory requirements.
We would only provide your personal information to a third party if it is necessary to perform our activities (i.e.if you have specific dietary requirements, we would provide that information to the organiser of the event).
Health information and other sensitive information
If you provide us with details of how you have been affected by brain cancer, including information about your medical condition, history andtreatment, this is considered health information. We will always seek your consent to the use and disclosure of such information, including using your story and image in our communications, social media and promotional material.
Research participants
If you participate in research programs that we conduct, we may collect personal information to record your involvement and to process the results of research and to contact you regarding participation in the study or future studies. The information we collect from you will generally be sensitive information because it will be your health information and could be other sensitive information such as information about your racial or ethnic origin. It will be handled in accordance with this privacy policy and any relevant research ethics approved by an external committee.
We may collect your personal information including:
• your medical history including, where relevant, a family medical history;
• your Medicare number and information about your privacy health insurance;
• current medications or treatments used by you;
• the name of any care provider, health service provider or medical specialist to whom we refer you back to or has referred you to us, copies of any referrals and reports;
• test results and samples.
Information may also be collected about individuals who are not research participants when we make a record about a research participant. For example, when collecting emergency contact details or a family medical history.
From time to time we may collate and analyse statistical data from information we have previously collected. In these cases, the data will be de-identified and aggregated before it is disclosed to third parties.
Biobank
As a brain cancer research organisation, we operate a biobank which stores biological samples and associated health data for use in research. Third party research organisations may provide us with samples and data from participants in their research studies, for inclusion in a biobank. We may use these samples and data to generate genetic or genomic information. Biobanks are a valuable resource to support research to develop new treatments, drugs and therapies and to understand health and disease conditions more broadly. We work with reputable contractors and third party service providers to operate our biobanks. Our biobank is designed and managed to protect the privacy of individuals and to comply with the highest standard of legal requirements and clinical ethics. In most cases, the biological samples and associated data are de-identified and it is not possible to identify individuals to whom the sample and associated data relates. Where this is the case, the samples and data will not be personal information which is subject to privacy laws. Where we do hold personal information in the biobank, it will be handled in accordance with this privacy policy and the relevant human research ethics approved by an external Human Research Ethics Committee. Research participants enrolled in this research will be given further information detailing how their personal information (including health information) will be handled.
How do we store your personal information?
Your personal information is stored onelectronic cloud-based databases and Microsoft Office 365. We also may hold hard copy information on-site at our office. We have implemented electronic and physical measures to protect the personal, sensitive and health information we receive from misuse, interference and loss, and from unauthorised use, modification or disclosure. We are not, however, liable for any unauthorised access or disclosure of information.
Your financial information
Our website uses Secure Sockets Layer (SSL) certificates to protect your credit card information over the internet. We also encrypt the credit card details we store on our electronic cloud-based database.
Access to and correction of your personal information
At your request, Charlie Teo Foundation will provide you with access to your personal information that is held by us. We may, however, refuse a request for access in certain circumstances in accordance with Australian Privacy Principle 12.
If you consider the personal information that we hold about you is inaccurate, incomplete, irrelevant or out-of-date, please contact us so that we can correct the information.
Unsubscribe
To unsubscribe from our e-mail database or opt-out of communications (including marketing communications), please contact us using the details below or opt-out using the opt-out facilities provided in the communication.
How are changes to this privacy policy made?
We may, at any time and at our discretion, change this Privacy Policy by publishing the amended Privacy Policy on our website. We recommend you check our website regularly to ensure you are aware of our current Privacy Policy.
For any questions or notices, please contact our Privacy Officer at:
Charlie Teo Foundation ABN 57 622 041 061
Phone: (02) 8880 8328
Email: info@charlieteofoundation.org.au
We will respond to requests within a reasonable timeframe.
Last updated December 2019