19 September 2023
Today we pay special tribute to our little friend Alegra. Today would have been Alegra’s 12th birthday. A beautiful angel, taken too soon, age six.
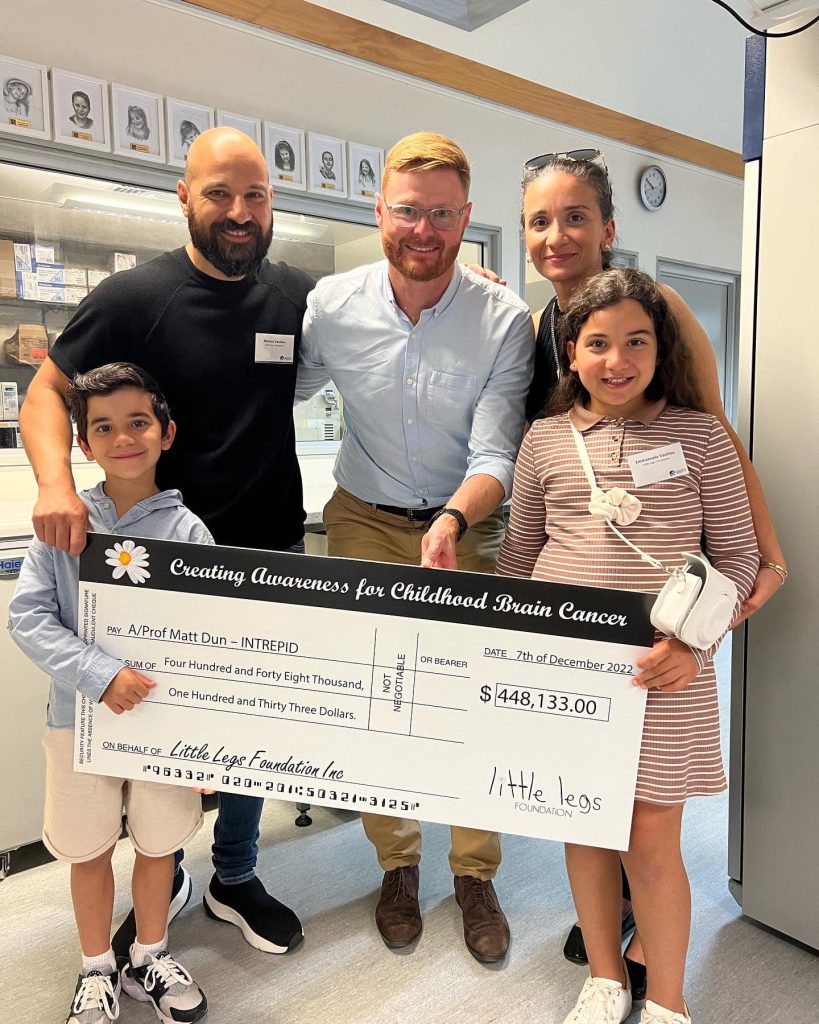
The Alegra’s Army Grant was established by the Little Legs Foundation in partnership with the Charlie Teo Foundation to ensure that no family and child has to suffer the ultimate price like Alegra.
We are proud today to honour Alegra by sharing recent DIPG research progress across the world.

Lethal, inoperable, and seemingly incurable – these are the sombre labels that have long characterised Diffuse Midline Gliomas (DMG), previously known as Diffuse Intrinsic Pontine Gliomas (DIPG).
DMG is a fatal type of cancer that predominantly affects children’s brain and spinal cords.
Unlike many other solid paediatric cancers, DMG doesn’t grow as large masses; instead, these cancer cells blend into healthy tissue, making them highly evasive and difficult to treat. The current treatment approach is palliative radiotherapy, bringing only short-lived relief, with patients often surviving just 9 to 11 months after diagnosis.
Here is where HOPE enters the picture….
Published findings from a team at Michigan University and international collaborators including Charlie Teo Foundation-funded superstar Professor Matt Dun, have shown for the first time in clinical trials that a new compound called ONC201 nearly doubled survival for patients with DMG compared to previous patients. This breakthrough cracks the seemingly unbreakable armour of DMG.
This breakthrough brightens the path ahead, reminding us that even in the face of the toughest challenges, science's light can guide us toward solutions we once thought were beyond our grasp.
Prof Dun’s team didn’t stop there… They also figured out how DMG becomes resistant to ONC201 and found a way to tackle it. By combining ONC201 with another drug, ‘paxalisib,’ and standard radiotherapy, they’re aiming to boost the treatment’s effectiveness. These preclinical findings generated by Prof Matt Dun and his University of Newcastle research team supported the rationale for a DMG clinical trial known as PNOC022 that was recently brought to Australia, to test this combination therapy in DMG patients. Read more

Through the Charlie Teo Foundation’s More Data grant scheme, Prof Matt Dun and his team have also uncovered that ONC201 can potentially empower the immune system to better recognise and attack DMG cells. Empowering and engineering the immune system to better recognise and attack cancer cells has been shown to be effective and even curative in some forms of leukemia. However, this strategy remains quite difficult to implement in solid tumours like DIPG for a plethora of reasons which have been recently summarized by Dun Lab superstar, PhD candidate Bryce Thomas (supported by an Alegra’s Army PhD Scholarship), in the prestigious journal Trends in Cancer.

One of the main reasons DMG is so hard to tackle is because the tumour creates an environment around itself that shields it from the body’s immune system. This means that the immune system, which normally fights off infections and diseases, can’t effectively recognise and attack the cancer cells. This protective shield is made up of certain cells that are meant to help us, but in this case, they end up aiding the cancer’s growth.
Preliminary findings from Prof Matt Dun’s Alegra’s Army Grant funded in partnership with the Little Legs Foundation has shown that ONC201 can potentially weaken this protective shield, making the DMG cells more visible to the immune system and promoting an influx of battle-ready immune cells into the tumour. Further validation of this work is currently underway as the lab perfect the best DMG model to study the phenomenon in the lab. The Dun Lab suggests that a possible alternative treatment can include the use of ONC201 in combination with another type of immunotherapy called adoptive cell therapy or a chimeric antigen receptor (CAR) T cell therapy. This innovative approach involves modifying a patient’s own immune cells, teaching them to specifically target the DMG cancer cells.

Preliminary evidence from a Stanford study has shown that this approach demonstrated enhanced tumour reduction and improved neurological conditions in three of four patients.
However, an ongoing challenge associated with this strategy involves teaching the cells what DMG cells look like because not every DMG cell looks alike. From this project, Prof Matt Dun’s team have identified a potential marker that can better identify and differentiate DMG cells from healthy cells. The group are currently working on a strategy to exploit the finding in the clinical setting.
In the end, this isn’t just about science—it’s about HOPE. Prof Dun and his team are at the forefront, driving progress and uniting the masses. Their ONC201 breakthrough brightens the path ahead, reminding us that even in the face of the toughest challenges, science’s light can guide us toward solutions we once thought were beyond our grasp.
This Childhood Cancer Awareness Month we’re shining a light on the need for better treatments.

Brain cancer research is significantly underfunded compared to other cancers, meaning survival rates have barely improved in about 40 years. Research funders like the Charlie Teo Foundation are crucial to changing the future for brain cancer patients and families.
To date Charlie Teo Foundation has committed more than $10 million to brain cancer research in Australia and globally. This includes $2.7 million awarded into DIPG/DMG specific research. Compare this to the Australian Government that has awarded $970,000 to DIPG/DMG specific research over that same period.
United together we can shine a bright light on the need for more funding for brain cancer research and better treatments in Australia.